Ageing is no longer something we can plan for someday; it is unfolding around us, quietly and steadily. Alongside this shift is a sharp rise in dementia, with an estimated 7.4% of Indians aged 60 and above living with the condition. Behind these numbers are millions of individuals and families navigating uncertainty, fear, and long-term care needs that cannot be met through short-term or fragmented solutions.
This is why dementia specialists matter. Dementia care cannot be improvised aimlessly; it demands informed, consistent, and skilled expertise. Dementia is far more than memory loss; it is a progressive condition that affects health, independence, relationships, dignity, and identity. Specialists bring the clinical insight, behavioural understanding, and ethical sensitivity needed to design care models that are sustainable, humane, and adaptable over time.
By centering care around deep expertise and personhood, sustainable elder care models in India can move beyond basic supervision to specialists who truly understand the condition and the complications it may bring along with it. Only then can we offer continuity, dignity, and meaningful quality of life at every stage of the dementia journey.
Dementia care is both Clinical and Communal
Dementia is not a single medical issue to be treated in isolation. It is a complex interplay of brain changes, chronic conditions such as diabetes and hypertension, mental health challenges, reduced mobility, and deeply human social needs. Caring well for someone with dementia, therefore, means holding all these threads together, accurate diagnosis, careful medication management, cognitive and behavioural support, physiotherapy and occupational therapy, caregiver guidance, and thoughtful planning for the future.
This is where specialist expertise makes a critical difference. Professionals trained in dementia bring the clinical insight and lived understanding needed to connect these dimensions into coherent, responsive care. When specialists are embedded within care models, the impact is tangible: dementia is identified earlier, medications are managed more safely, falls and behavioural distress are better prevented, and rehabilitation is tailored to the individual. Just as importantly, care becomes more consistent, more compassionate, and more aligned with the person’s dignity and daily life, strengthening not only clinical outcomes, but the entire care community around the elder.
India faces a specialist gap, and that gap threatens scale
Building dementia care that can truly meet India’s growing needs is not just a question of intent, but of expertise. The country’s pool of trained geriatricians, dementia specialists, and multidisciplinary care teams remains far smaller than what an ageing population demands. Approximately 75% of India’s elderly suffer from at least one chronic disease, and 23.3% experience multimorbidity, which requires ongoing medical oversight and specialist involvement. This is a number that calls out the need for more elder care specialists. A
Without sustained investment in specialist training and in expanding distributed expertise, care continues to be concentrated in a handful of urban centres. 74% of doctors are located in urban areas that serve only about 28% of the population, indicating a major rural gap in access to medical professionals.
This leaves rural and semi-urban families largely unsupported, often forcing them to navigate complex care decisions on their own. The consequences are far-reaching: caregiver exhaustion, delayed or inadequate treatment, avoidable hospitalisations, and inefficient reliance on tertiary healthcare systems. Closing the specialist gap is therefore not optional; it is foundational to building dementia care that is equitable, sustainable, and truly accessible across India.
Specialists are the glue for multidisciplinary, sustainable models
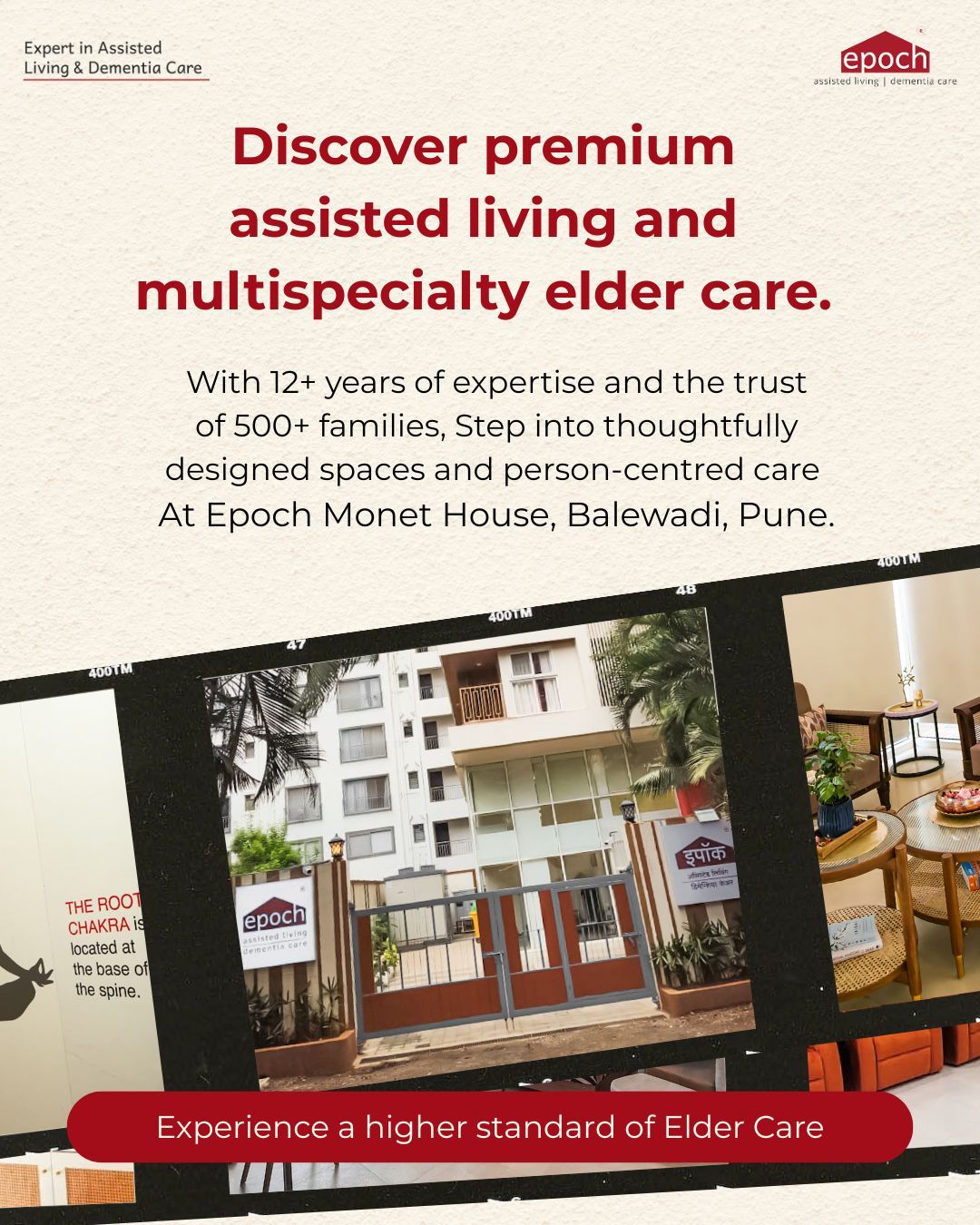
Sustainable elder care models, whether residential assisted living, integrated community care, or hospital-linked memory clinics, work best when a dementia specialist serves as the clinical anchor. Their presence brings structure, consistency, and depth to care, ensuring that systems can scale without losing quality or compassion. Here is what specialist leadership makes possible:
- Clinical leadership for multidisciplinary teams.
Dementia care depends on close coordination between doctors, nurses, physiotherapists, occupational therapists, social workers, and counsellors. Dementia Specialists will help guide diagnosis and care pathways, manage complexity, and ensure timely escalation, so everyone works toward a shared, person-centred plan.
- Standardised protocols and quality oversight.
Specialists design and continuously review protocols for medication management, behavioural symptom support, fall prevention, and end-of-life care. This reduces risks such as polypharmacy, improves safety, and creates measurable quality standards essential for long-term sustainability.
- Training and capacity building.
Through workshops, tele-mentoring, and on-site supervision, specialists upskill nurses, primary care doctors, and community health workers. This approach extends specialist knowledge far beyond individual facilities, strengthening care delivery across regions.
- Integration with tertiary healthcare services.
Specialist-led models connect seamlessly with hospitals for neurology, psychiatry, and diagnostic services. Elders gain timely access to advanced care without unnecessary transfers, lowering costs, reducing stress, and preventing avoidable complications.
Together, these elements transform dementia care from a series of isolated interventions into a resilient, well-coordinated system, one that can truly support elders and families over the long course of the condition.
Economic and human arguments align: How early interventions lower long-term costs
Dementia places a heavy and often invisible economic burden on families and healthcare systems, through repeated hospitalisations, poorly managed chronic conditions, and the loss of productivity when family members step away from work to provide care. When dementia is addressed late or without specialist guidance, these costs compound over time, both financially and emotionally.
Early involvement of dementia specialists changes this trajectory. Timely diagnosis, expert medication management, and structured functional rehabilitation can slow decline, prevent avoidable hospital admissions, and help elders maintain independence for longer. The result is not only better clinical outcomes, but meaningful cost savings over the long term.
Seen through this lens, investing in specialist roles, such as memory clinic leads, dementia nurse specialists, and geriatric physiotherapists, is not an added expense, but essential care infrastructure. Evidence from global and national analyses consistently shows that dementia’s economic burden is vast, and that early, expert-led interventions deliver measurable returns by reducing crisis-driven care and supporting more sustainable, dignified ageing.
Challenges that we face in creating sustainable elder care models in India
Building sustainable elder care models in India comes with its own set of complex challenges:
- Deep-rooted stigma and denial
Dementia and cognitive decline are often dismissed as “normal ageing.” Families delay seeking help due to shame, fear, or lack of awareness. This postpones diagnosis and pushes care into crisis mode.
- Crisis-driven decision-making
Most elder care decisions happen after a fall, hospitalisation, behavioural episode, or burnout of a primary caregiver. There is very little culture of early planning or preventive intervention.
- Cost sensitivity and short-term thinking
Long-term care is often seen as an avoidable expense rather than a necessary investment. Families may hesitate to commit to structured care until risks escalate, which ultimately increases overall burden and cost.
- Inconsistent training of frontline caregivers
Many caregivers enter the workforce without structured training in dementia-informed practices, behavioural management, or communication techniques, leading to reactive or inconsistent care delivery.
- Fragmented medical documentation and continuity gaps
Medical records are often scattered across hospitals, clinics, and home care providers. Lack of standardised tracking makes it difficult to monitor disease progression or coordinate long-term care plans effectively.
Shifting the focus toward early, specialist-led intervention is essential. Dementia specialists can ensure that training is accurate and relevant, that medical documentation is clear and meaningful, and that the right information reaches families, caregivers, and the wider community. Their leadership anchors the system in expertise, enabling elder care models to move from reactive responses to thoughtful ones.
Conclusion: Specialist care is not optional; it’s foundational
Dementia is a clinical, social, and systems-level challenge. For India to build elder care models that are humane, affordable, and truly scalable, dementia specialists must sit at the centre of both design and delivery, not on the margins. Their expertise provides clinical leadership, strengthens multidisciplinary teamwork, and expands reach through training and tele-enabled care models. Investing in specialist capacity today is not an indulgence; it is the most practical and responsible path to building robust elder care systems for the millions who will need them in the years ahead.