Diabetes and dementia are two prevalent health conditions that have been the focus of extensive research in recent years. While each condition has its own distinct characteristics, emerging evidence suggests a strong correlation between diabetes and an increased risk of developing dementia. As Head of Learning at Epoch Elder Care, an assisted senior living facility, I am deeply committed to promoting preventive health measures. Through this blog, I will delve into the correlation between diabetes and dementia, exploring the shared risk factors and the vital role of lifestyle choices in preventing these conditions. Join me on this journey to uncover the best strategies for optimal brain health and well-being, especially for elders.
Understanding the Correlation:
-
Impact of High Blood Sugar Levels on Brain Health
Chronic hyperglycemia promotes cognitive decline through glycation, where excessive sugar molecules react with brain proteins, forming harmful compounds that negatively affect brain tissue and cognitive function. Maintaining stable blood sugar levels is vital to safeguard cognitive abilities and reduce the risk of neurodegenerative conditions.
-
Insulin Resistance and Cognitive Decline
Insulin resistance and impaired signaling are linked to dementia and cognitive decline, affecting brain cells and increasing vulnerability to neurodegenerative processes. Insulin plays a crucial role in brain health and neuroprotection, emphasizing the importance of maintaining proper sensitivity to support cognitive function and reduce the risk of cognitive disorders.
Shared Risk Factors:
Age as a Common Risk Factor
Advancing age is a shared risk factor for diabetes and dementia, leading to higher prevalence in older adults. Age-related changes in insulin sensitivity and brain function are crucial in this relationship, and the cumulative effects of long-term diabetes can significantly impact cognitive health in the elderly, potentially contributing to cognitive decline and neurodegenerative diseases
Genetic Predisposition
Genetic predisposition significantly influences the development of diabetes and dementia, with strong familial links and shared genetic factors involved in these conditions. Specific gene variants associated with both diseases highlight the impact of shared genetic pathways on metabolic regulation and brain function.
Vascular Health and the Diabetes-Dementia Connection
Diabetes profoundly affects blood vessels and the brain's vascular system, leading to microvascular complications that contribute to cognitive impairment. The interplay between diabetes, hypertension, and cerebrovascular disease increases the risk of dementia, as these conditions collectively harm the brain's blood supply and overall vascular health.
Alzheimer's Disease and Diabetes: A Key Link
(Alzheimer's disease is a specific type of dementia, characterized by progressive memory loss and cognitive decline.)
Diabetes (specially Type 2) and Alzheimer's disease have a bi-directional relationship, with insulin resistance promoting amyloid beta and tau pathology in the brain. Common pathophysiological mechanisms suggest that addressing one condition may impact the management or prevention of another. Diabetes is also associated with structural and functional brain changes, leading to cognitive decline. It affects hippocampal integrity, memory function, and executive abilities, primarily due to disruptions in glucose metabolism and cerebral energy utilization.
What non-pharmacological measures can be employed to manage and mitigate the risk of developing diabetes and dementia?
According to various researches, dietary and lifestyle changes can help to avoid neurodegeneration and promote brain health. Enhancing blood glucose levels may aid in both the prevention and treatment of dementia.
We should aim to adopt a dietary approach that promotes stable blood sugar and insulin levels (low glycemic), while also minimizing inflammation and providing essential nutrients for optimal brain health.
The following are tips for proper nutrition that should be considered in elder care:
- Small amounts of nutrient-rich carbohydrates like sweet potatoes, steel-cut oats, buckwheat, etc.
- Whole, unprocessed foods like vegetables, legumes, nuts, etc.
- Whole fruits per day for at least two days in a day
- Use of high-quality oils such as cold-pressed olive oil and oils of nuts and seeds
- Omega-rich foods twice a week
- High-protein foods that can be animal- or plant-sourced
- 8–10 servings of non-starchy vegetables in a day
Apart from that, there are many nutrients that are essential for the brain and its cognitive function. They are as follows:
- Vitamin A (Essential for neurogenesis and resiliency of the brain)
- Vitamin C (essential for the growth of neurons, the formation of the myelin sheath, and neurotransmitter synthesis)
- Vitamin D (essential for cognitive function)
- Vitamin E (which protects cells from oxidative stress and may help prevent or delay cognitive loss)
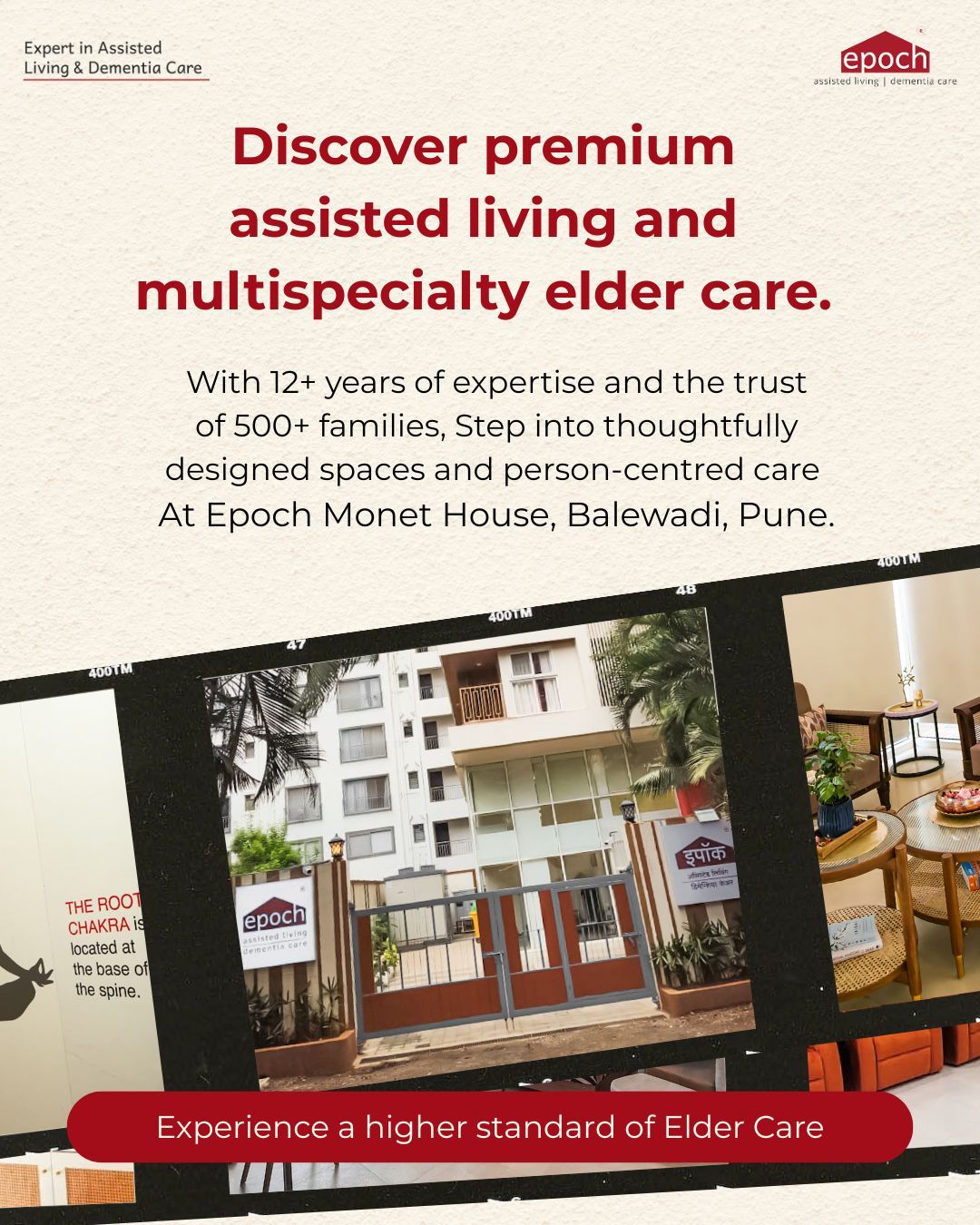
At our Epoch Elder Care Facilities, we offer a comprehensive cyclic menu tailored for the elderly, with both vegetarian and non-vegetarian options. Our small, intermittent meal approach fosters better digestion and nutrient absorption. For residents with diabetes, we provide a specialized diabetic diet with low glycemic foods and careful sugar monitoring. We are dedicated to promoting the health and well-being of our elderly residents through nutritious and delicious meals tailored to their needs and preferences.
- Monitoring of Blood Glucose Levels
Blood glucose monitoring is essential in managing diabetes, enabling regular tracking of blood sugar levels. Using a glucose meter, a small blood sample is analyzed, helping individuals understand their body's response to food, activity, and medications for informed decisions. Regular monitoring empowers diabetes management, leading to personalized treatment plans for better health outcomes.
Regular blood glucose monitoring is crucial for elderly individuals with diabetes. To minimize discomfort, we rotate testing sites and follow the doctor's advice on frequency. Periodic HbA1c testing enhances accuracy, ensuring effective diabetes management for our elderly residents' health and well-being.
When a body is under chronic stress, it releases hormones that can increase blood glucose level. Apart from the fact that stress causes inflammation of the brain cells, According to a study published in the Alzheimer's & Dementia Journal, brain inflammation is a significant neuropathological route that is relevant to the cognitive decline brought on by Alzheimer's disease.
At Epoch, we firmly believe in the power of engaging activities to prevent stress and promote well-being in individuals with diabetes and dementia. As one of our activities, we thoughtfully plan "Movie Time" on Sundays, featuring movies from their era, which serves as an effective stress-relieving activity. By immersing our elderly residents in the nostalgia of familiar films, we create an emotionally comforting environment, which can reduce anxiety and tension.
A study of the literature turned up 27 studies looking at how exercise affects cognitive performance in adults above 60 years. A strong correlation between physical activity levels and cognitive function was found in 26 of the investigations, indicating that exercise may be a useful strategy to slow down cognitive aging.
At our Epoch homes, we prioritize the well-being and physical health of our residents at all levels. In our setting, our dedicated caregivers provide support by assisting residents in both active and passive exercises, tailored to their individual needs and abilities. Additionally, our in-house physiotherapists play a crucial role in conducting personalized physiotherapy exercises, both one-on-one and in group sessions, to enhance mobility, flexibility, and overall physical function. This comprehensive approach ensures that our residents receive the specialized care they require, promoting their independence and improving their overall quality of life.
According to a recent study in the journal PLoS (Public Library of Science) Medicine, those over 50 years old who sleep less than five hours a night are more likely to acquire numerous chronic conditions like diabetes and cardiovascular diseases.
At Epoch, we recognize the importance of proper sleep for the well-being of our elderly residents. To address circadian rhythm disturbances, we actively engage them in a variety of activities and exercises within our facility. By providing a stimulating and fulfilling environment, we aim to promote a healthier sleep-wake cycle and improve their overall sleep quality. This approach not only enhances their physical and mental health but also contributes to a more vibrant and fulfilling lifestyle during their stay at our facility.
Besides the non-pharmacological approach, we adhere to the drug/insulin regimen as prescribed by the endocrinologist.
To Sum Up
Regular blood glucose monitoring, prescribed medications, balanced diet, physical activity, brain-stimulating activities, stress reduction, social interactions, and emotional support are vital in managing diabetes and dementia holistically. With this comprehensive approach and with proper treatment and guidance from specialists (like endocrinologists and neurologists), we can address physical, mental and emotional aspects, optimizing brain health, preventing complications, and improving the quality of life for individuals with these conditions.